48.4 million Americans lack adequate access to a pharmacy

Mark Winfrey // Shutterstock

Mark Winfrey // Shutterstock
48.4 million Americans lack adequate access to a pharmacy
Pharmacies and pharmacists play a critical role in our healthcare system. They dispense prescription and over-the-counter medications, provide immunizations, and counsel patients on medication side effects, interactions, and regimens.
These essential services ensure patient safety and help patients take their medications as prescribed, ultimately improving the overall health of our communities.
In an ideal world, everyone would have convenient access to necessary health services like pharmacies. But this isn’t the case. And with many pharmacies closing, the problem is only getting worse. In fact, over the past five years, more than 1,300 pharmacies have closed, leaving 48.5 million people—a significant jump from 41.2 million in 2021—without nearby access to a retail pharmacy, GoodRx reports.
These pharmacy deserts exist in counties big and small, extend across the country, and will likely become more widespread as pharmacies continue to close.
Key takeaways:
- Pharmacy deserts are expanding rapidly, leaving 1 in 7 Americans without easy access to a pharmacy. Over 48.4 million people now live in areas where filling a prescription requires a lengthy drive.
- As pharmacy closures accelerate, more Americans are facing longer drive times, fewer opportunities to comparison-shop for medication prices, and greater challenges in filling their prescriptions.
- In pharmacy desert counties, residents face an increase in both travel time and distance. On average, those in nonmetropolitan areas must drive 85 minutes and cover 36 miles, while metropolitan residents travel 53 minutes and 18 miles (round trip).
- More than 1 in 4 metropolitan counties and over half of nonmetropolitan counties are classified as pharmacy deserts. Rural states like Alaska, Montana, Nebraska, and the Dakotas are among the hardest hit.
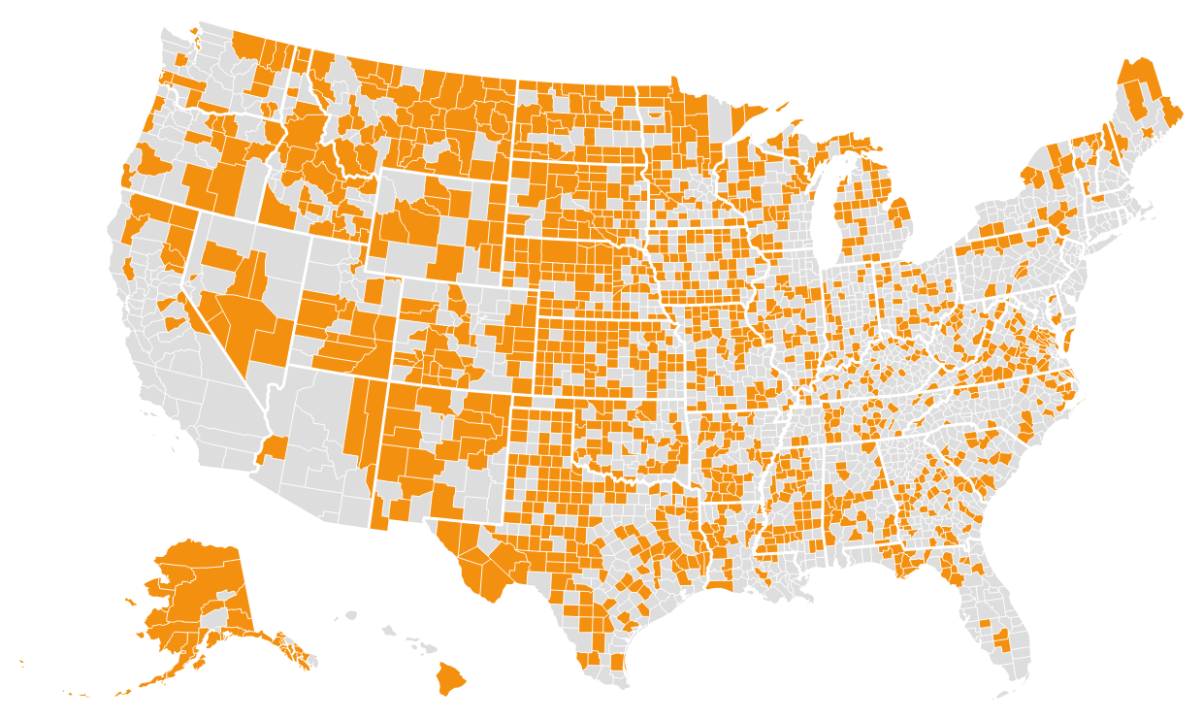
45% of U.S. counties are pharmacy deserts
Today, 48.4 million people, or 1 in 7 Americans, live in a pharmacy desert.
GoodRx Research identified pharmacy deserts by comparing the average driving distance to nearby pharmacies to the average time it takes to drive 10 miles in a rural area (about 15 minutes). We based our formula on the U.S. Department of Agriculture (USDA) definition of food deserts.
The below map shows areas where residents have to drive more than 15 minutes to the nearest pharmacy—a distance that can make it difficult to fill a prescription. The farther a person lives from a pharmacy, the less access they have to in-stock medications and different pharmacies for price-shopping (since prices for the same medication often vary across pharmacies). Explore county-level detail in the interactive version of this map at GoodRx.com.
GoodRx
Where pharmacy deserts are most prevalent
Pharmacy deserts are spreading across both metropolitan and nonmetropolitan areas, but the burden is not distributed evenly. In nonmetropolitan areas, residents face particularly severe challenges, with average round-trip travel times of 85 minutes and distances of 36 miles to reach a pharmacy. Meanwhile, those in metropolitan pharmacy deserts experience shorter, yet still significant, average round-trip drives of 53 minutes covering 18 miles.
Certain states have an especially high share of counties that are pharmacy deserts, including:
- Alaska: 82%
- North Dakota: 81%
- Montana: 79%
- South Dakota: 74%
- Nebraska: 70%
- Kansas: 68%
- Wyoming: 61%
While these states face widespread pharmacy shortages, specific counties across the U.S. also highlight the extreme challenges some communities experience. In Arizona’s Navajo County, over 118,000 residents must travel more than 100 minutes round trip, on average, to reach the closest retail pharmacy. In neighboring Apache County, 87,000 residents face even greater difficulties, with average travel times exceeding three hours. These prolonged travel times create logistical barriers and also limit residents’ ability to price-shop for medications or find in-stock prescriptions—challenges that are becoming more common as pharmacy closures accelerate nationwide.
As pharmacy deserts continue to expand, these disparities in access are likely to deepen, leaving millions of Americans struggling to fill their prescriptions in a timely and affordable manner.
States hit hardest by pharmacy closures
While pharmacy deserts have expanded across the country, some states have been hit particularly hard by pharmacy closures in recent years. Between 2021 and 2024, several states have seen significant declines in pharmacy access, leaving millions more residents without a nearby option for filling prescriptions.
Ohio has experienced the most dramatic shift in pharmacy access. Ohio’s pharmacy desert population has grown by 410,000, reaching nearly 2 million—up from 1.6 million in 2021. North Carolina follows closely behind, with pharmacy closures affecting nearly 1 million additional residents.
In the western U.S., Oregon and Washington have both seen pharmacy deserts expand rapidly, particularly in rural and suburban areas. Oregon’s pharmacy desert population has increased by 337,000 between 2021 and 2025, rising from 600,000 to 937,000 (a 56% increase in their pharmacy desert population). Washington has faced similar challenges, with closures disproportionately impacting lower-income and Native American communities.
Meanwhile, Michigan and Pennsylvania have experienced growing disparities between urban and rural pharmacy access, with some smaller towns losing their last remaining pharmacies. California, despite its large number of urban centers, has also seen worsening access in its rural regions, particularly in the Central Valley and northern parts of the state.
Who is most affected by pharmacy deserts?
Certain demographics are disproportionately impacted by the rise in pharmacy deserts. On average, nearly 9 in 10 people living in a pharmacy desert are in a rural area. Overall, more than half (56.8%) of all rural residents live in a pharmacy desert, highlighting the significant gap in pharmacy access outside urban centers.
Older adults are also disproportionately affected. In the average pharmacy desert, more than 1 in 5 residents (22.3%) in pharmacy deserts are 65 years old and older (Medicare-age), compared to 19.1% in non-desert areas. As this population often relies on multiple prescriptions to manage chronic conditions, limited pharmacy access poses an even greater challenge.
There are also racial and ethnic disparities, with some communities facing greater barriers than others. In pharmacy deserts, the average percentage of American Indian and Alaska Native residents is significantly higher than in non-desert areas (3.7% versus 1.4%), reflecting the longstanding healthcare access challenges in many tribal and rural regions. Meanwhile, Latino (9.4% versus 11.2%) and Asian (0.9% versus 2.4%) populations are underrepresented on average in pharmacy deserts compared to non-desert areas.
Economic factors further exacerbate disparities. The median household income in the average pharmacy desert is notably lower at $59,633, compared to $66,184 in non-desert areas. Additionally, the percentage of uninsured adults is higher in the average pharmacy desert (14.4% versus 12.9%), making it even harder for residents to afford their medications.
As pharmacy closures continue, millions of Americans face even greater barriers to accessing essential medications. Addressing these growing pharmacy deserts will require targeted solutions to ensure that all individuals—regardless of geography, income, or demographics—can obtain the prescriptions they need without excessive travel times or financial burdens.
The bottom line
Despite the growing need for prescription medications, pharmacies are becoming increasingly scarce for millions of Americans. Fewer pharmacies mean longer drive times as well as longer wait times at the pharmacy counter. These additional barriers to medication access can negatively affect health outcomes as it becomes more challenging for people to fill and take their prescription medications. Unfortunately, the spread of pharmacy deserts is not slowing.
As more pharmacies disappear, policymakers, healthcare professionals, and communities will need to find new ways to ensure people can access the medications they need. Expanding mail-order pharmacy options, allowing pharmacists to provide a wider range of healthcare services, and investing in telehealth solutions could help bridge the growing gaps in pharmacy access. Without action, millions more Americans may soon find themselves living in a pharmacy desert.
This story was produced by GoodRx and reviewed and distributed by Stacker.
![]()



