Urban vs. rural prescription costs: How geography shapes spending

oasisamuel // Shutterstock
Urban vs. rural prescription costs: How geography shapes spending
Where you live can shape your health and your prescription costs. Urban and rural communities differ not just in lifestyle and resources, but also in the medications people take and how much they pay for them out of pocket.
New research from GoodRx, a platform for medication savings, shows that geography influences things like whether patients use newer, brand-name therapies and how much they pay to manage chronic conditions. This research underscores a stark divide — where you live could change the course of your care.
Key takeaways:
- Where you live plays a significant role in healthcare access and spending.
- Residents in urban areas spend more out of pocket and use more brand and specialty drugs than their rural counterparts, who tend to use more affordable generics and older treatments.
- This urban-rural divide in healthcare spending and use may reflect the disparate geographic distribution of healthcare professionals and specialists as well as differences in insurance coverage and cost sensitivity.
Understanding the urban-rural divide
Urban counties are typically defined as areas with larger populations (at least 50,000 people), or where at least 10% of the population commutes to an urban county. Rural counties, on the other hand, include suburban areas with smaller populations, or counties where residents generally commute to smaller (“micro”) areas, and areas with the most limited population sizes and where commuting residents may travel to a small town (9,999 or fewer people) for work.
Researchers have found that people living in rural areas tend to face more health challenges than those living in urban areas, including higher rates of chronic disease and stroke. In comparison, people living in urban areas may face different but equally complex challenges, such as asthma tied to environmental pollutants or structural barriers to healthcare created by gentrification and uneven health systems.
GoodRx identified nine conditions that have large differences in out-of-pocket expenditures for urban versus rural populations. Below, delve into these gaps in spending and access across the geographical divide.
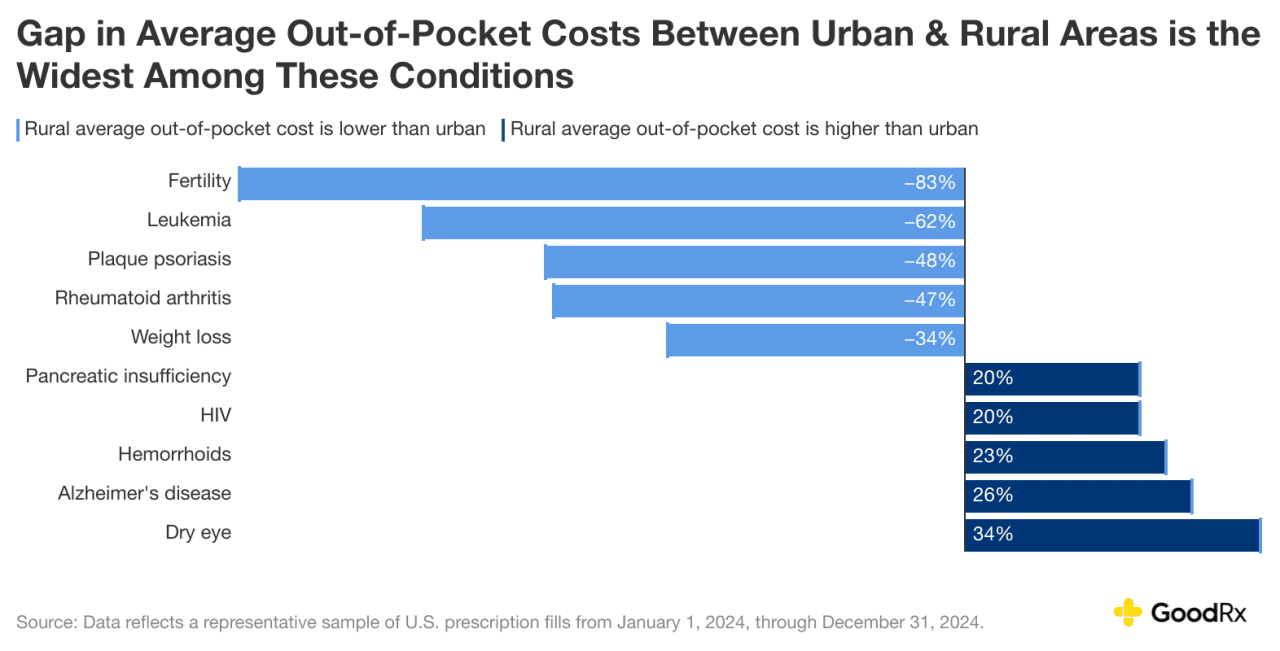
Certain conditions see the widest prescription-spending gaps across urban and rural areas
On average, people in rural areas spend about half as much out of pocket on prescriptions compared to urban residents ($38 versus $79 per fill, respectively). But people in rural areas actually face higher out-of-costs prescription costs to treat certain conditions.
Residents in urban versus rural areas don’t always face wide-scale gaps in out-of-pocket prescription expenditures. But the gap is notable for some treatments, such as fertility medication. People living in rural areas spend 83% less on fertility medication than people living in urban areas. One likely reason for this is utilization and access. A study published in 2016 examining fertility outcomes in women of reproductive age in Georgia found that compared to women living in urban areas, women in rural areas were 11% less likely to see a doctor for fertility treatment.
On average, people living in rural areas also tend to pay less out of pocket for medications to treat these conditions:
- Leukemia (62% less)
- Plaque psoriasis (48% less)
- Rheumatoid arthritis (47% less)
On the other hand, people from rural areas tend to spend more on medications for the following conditions:
- Pancreatic insufficiency (20% more)
- HIV (20% more)
- Hemorrhoids (23% more)
- Alzheimer’s disease (26% more)
- Dry eye (34% more)
People in rural areas also spend 34% less out of pocket on weight loss medications.
GoodRx
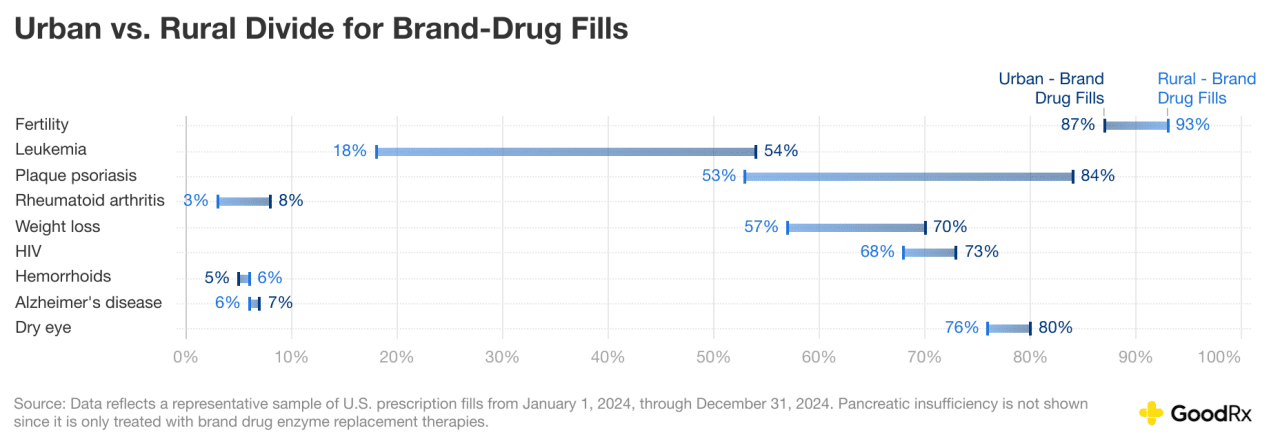
Rural areas rely more on generics and traditional treatments compared to urban areas
The gap in out-of-pocket prescription spending between urban and rural areas is only one part of the story. Across the nine conditions we analyzed, there are striking differences in the geographic areas that fill older, lower-cost generics versus newer, brand-name therapies. For seven of the nine conditions researchers looked into, people in urban areas are filling a larger share of brand medications, which often require specialist oversight, compared to people in rural areas. And the differences can be stark.
When it comes to leukemia medications, for example, people living in urban areas fill brand drugs three times more (over the course of a year) than people living in rural areas. Similarly, people in urban areas fill 30% more brand drugs for psoriasis and 13% more weight-loss brand medications than people in rural areas.
There are several reasons why people in rural areas may be less likely to fill brand drugs for some conditions than people in urban areas:
- Concentration of healthcare specialists: There’s a larger concentration of specialists in urban areas compared to rural areas. And many targeted biologics and speciality medications are brand medications, which require follow-up with specialists.
- Insurance coverage: Rural residents tend to have insurance with narrower coverage, such as Medicaid. And this can limit access to expensive brand medications.
- Cost sensitivity: Median household incomes are lower in rural areas compared to urban areas. People living in rural areas may have less disposable funds to spend on more expensive brand medications.
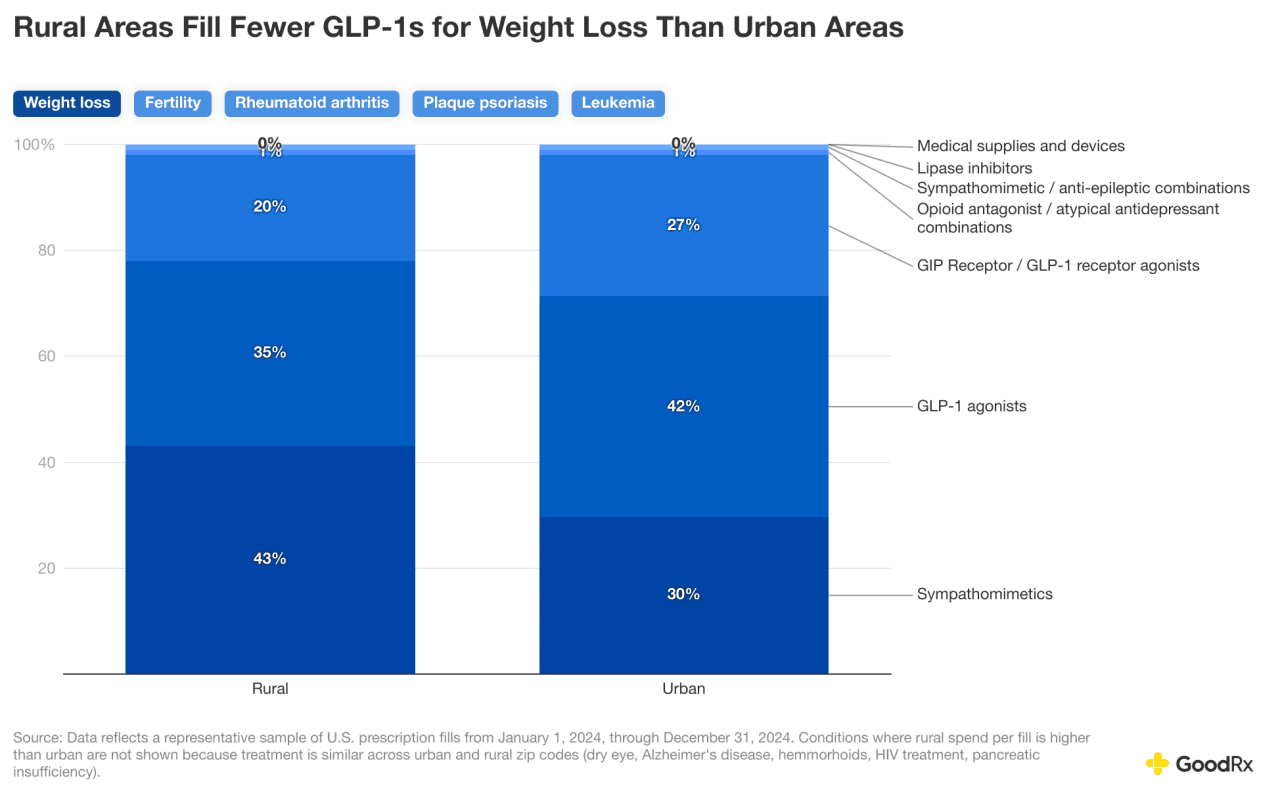
The difference in use of brand versus generic medications isn’t just a spending gap issue. Access to novel therapies can impact health outcomes as well. For example, glucagon-like peptide-1 (GLP-1) receptor agonists are a newer treatment for Type 2 diabetes and weight loss that have surged in popularity in recent years. Despite their popularity and effectiveness, GLP-1s lack widespread coverage under insurance plans.
For some conditions, such as Alzheimer’s disease and hemorrhoids, treatment typically relies on well-established generic medications that are widely used in both urban and rural areas, resulting in relatively low overall brand-drug prescription fills.
GoodRx
Weight loss
When it comes to weight loss, GLP-1s are a newer class of medications that include Wegovy and Zepbound. These are filled less frequently in rural zip codes. In contrast, older and/or generic medications, such as phentermine, make up a larger share of weight-loss prescriptions in rural areas. This disparity may reflect differences in healthcare provider access, insurance coverage, cost sensitivity, or clinical adoption of newer therapies.
GoodRx
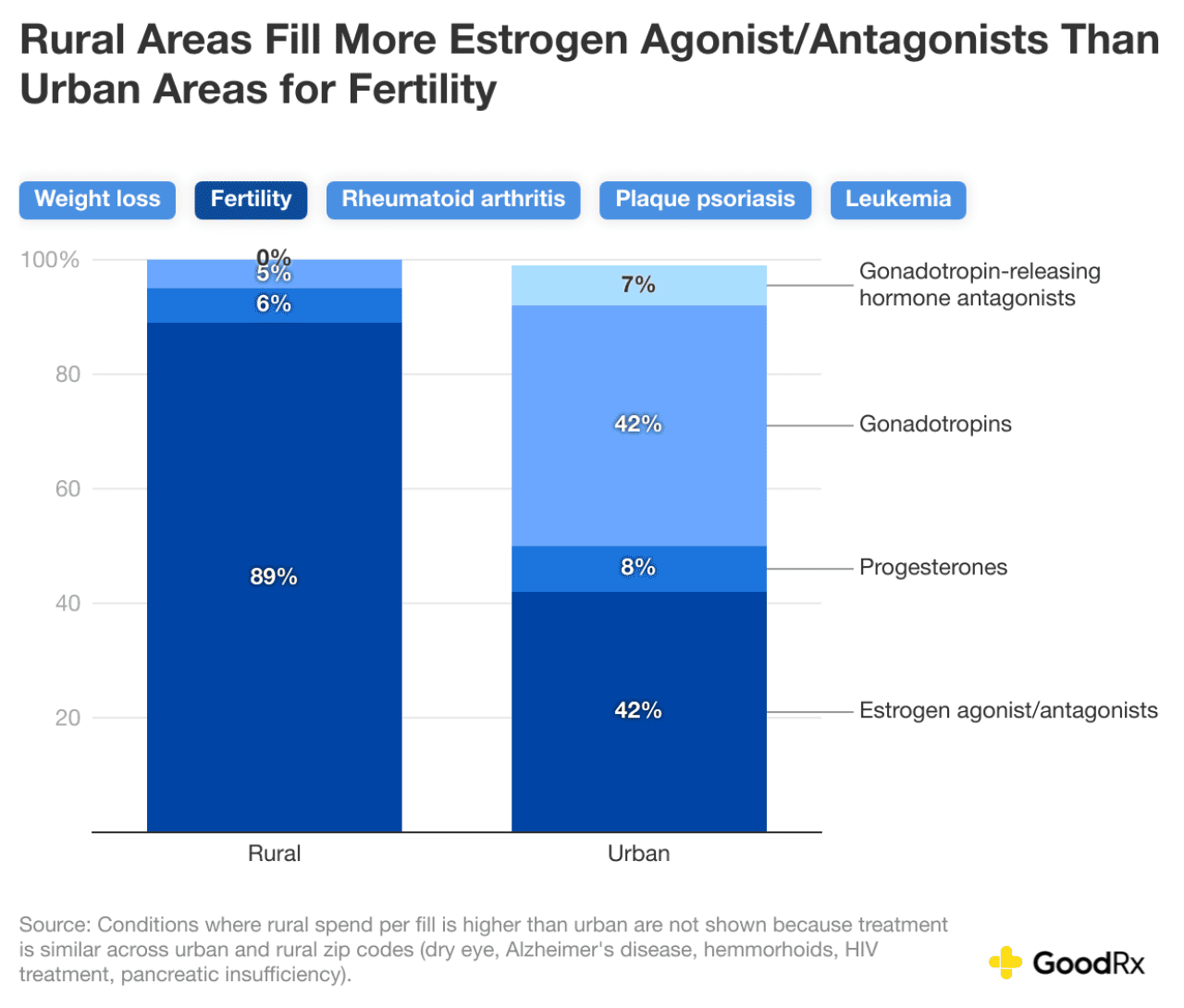
Fertility
Higher rural use of estrogen agonist/antagonists for fertility likely reflects limited access to fertility specialists and advanced treatments or cost constraints. Women in urban areas may be more likely to use assisted reproductive technology (ART), such as in vitro fertilization (IVF), to achieve pregnancy. An estimated 25 million women in the U.S. live in areas without nearby ART facilities, significantly limiting access to reproductive specialists for underserved rural or low-resource communities.
GoodRx
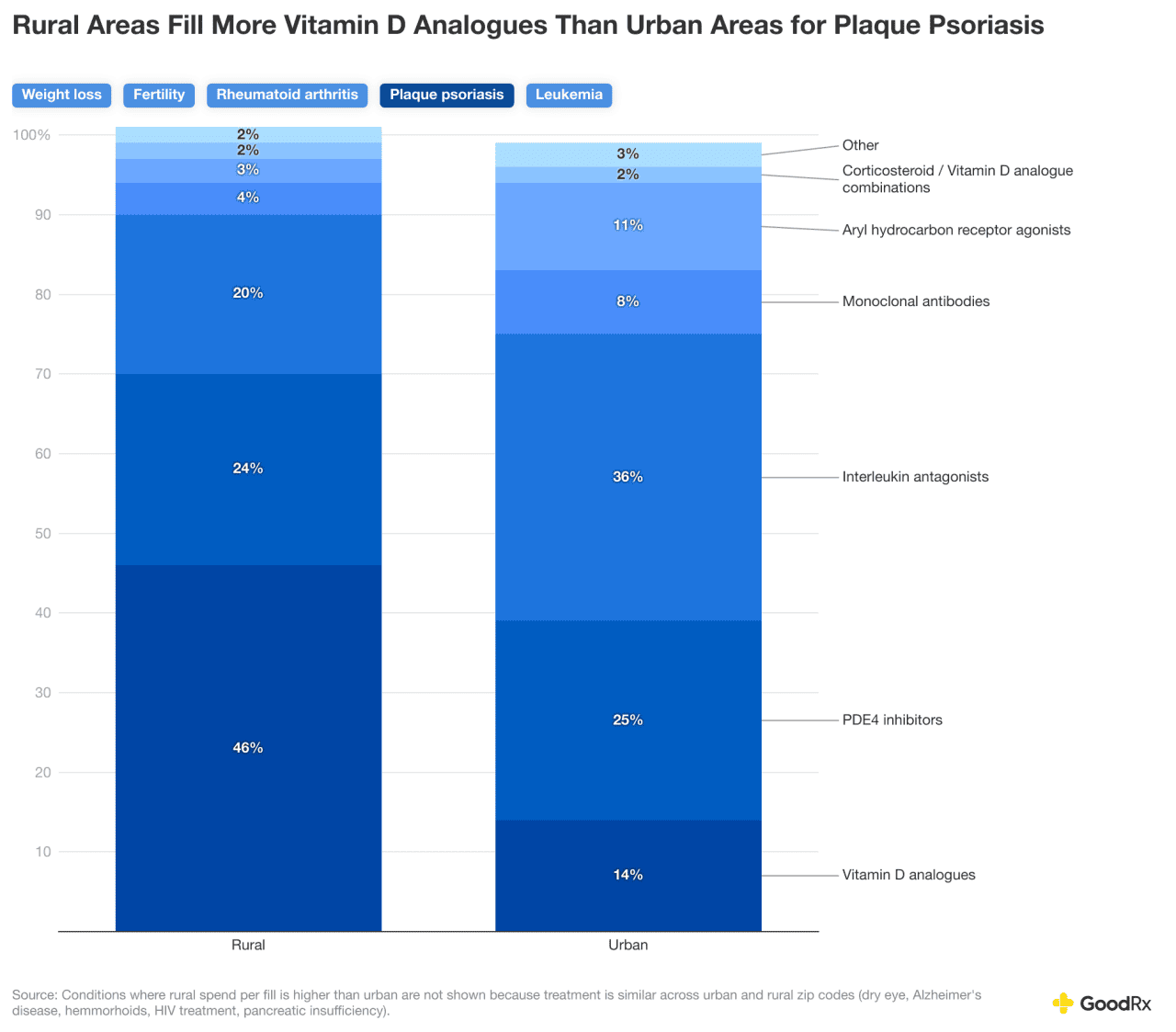
Plaque psoriasis
In rural areas, the most commonly prescribed medication for plaque psoriasis is calcipotriene, which is available in various topical forms. Insurance and cost barriers may lead to lower usage of other treatments. Adoption and implementation of newer medications may also be more prevalent in urban areas with higher concentrations of dermatologists. Zoryve and Vtama are two examples of topical treatments for plaque psoriasis that came to market in the last three years; they are filled more commonly in urban areas than rural areas.
GoodRx
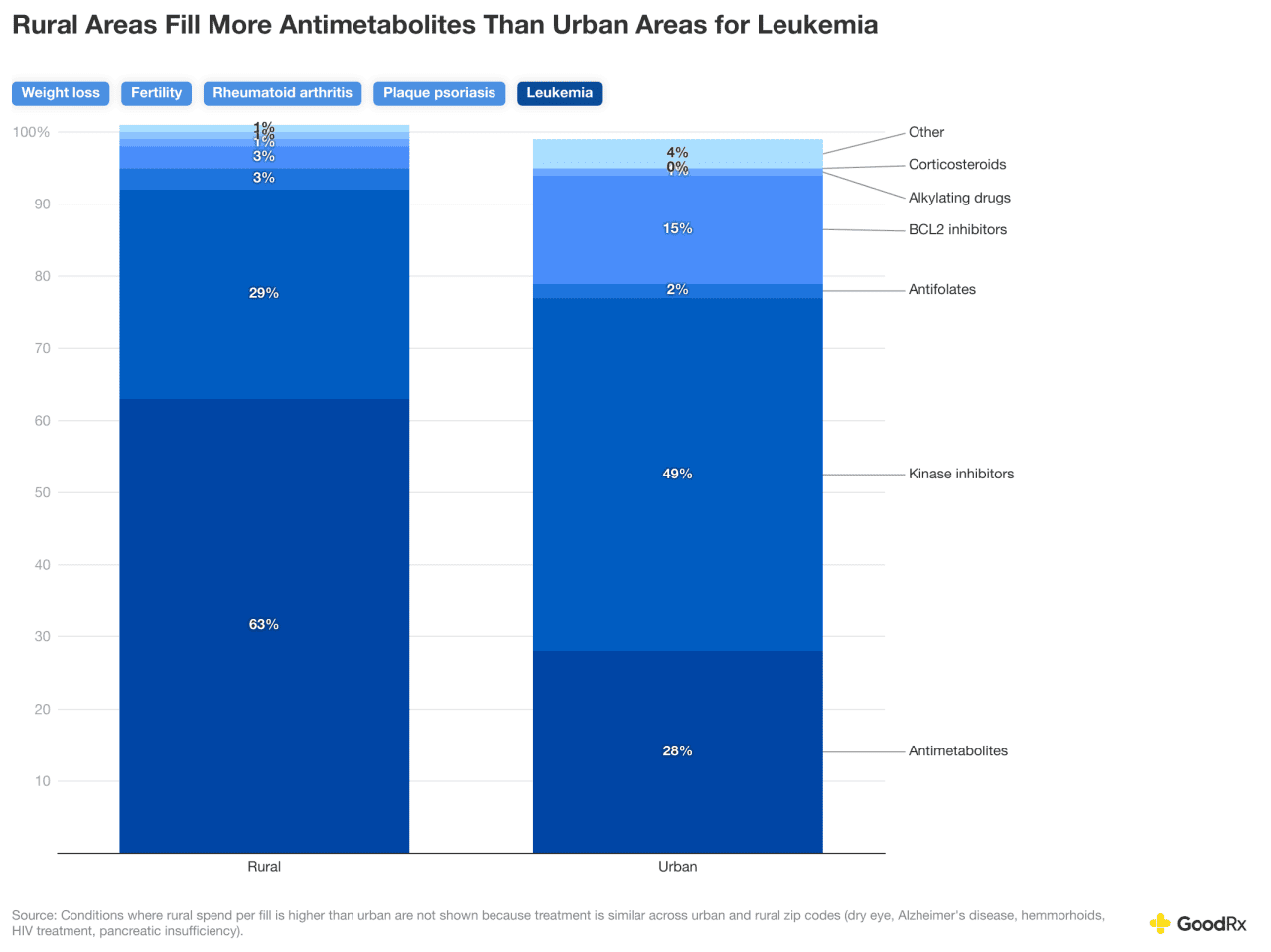
Leukemia
Antimetabolites are frequently used in oral maintenance therapy for leukemia. They can often be prescribed and managed in outpatient settings by nonspecialists or general oncologists, making them more accessible in rural areas. Antimetabolites are typically lower cost and generic, reducing both out-of-pocket costs and administrative hurdles. Urban areas are more likely to have access to specialty cancer centers, clinical trials, and novel targeted therapies, resulting in a greater percentage of fills for medications that are not antimetabolites.
GoodRx
The bottom line
Where you live doesn’t just determine your scenery; it can shape your health and expenses. Overall, people in urban areas have higher out-of-pocket costs and greater use of brand and specialty drugs, while those in rural areas rely more on generics and older treatments. There isn’t a singular cause of the urban-rural divide. There are likely several factors at play, including the higher concentration of healthcare specialists in urban areas and narrower insurance coverage for people living in rural areas.
Rural residents tend to use more affordable, established medications, while urban residents access newer, costly therapies that often require specialist follow-up. There’s also evidence of geographic disparities in costs for treating chronic conditions, making universal affordability and access difficult.
Methodology
Out-of-pocket costs: Researchers calculated total out-of-pocket costs using a representative sample of U.S. prescription fills from Jan. 1, 2024, through Dec. 31, 2024. Amounts paid were normalized based on the dispensed quantity to a 30-day supply.
Condition-level spending was estimated by analyzing drug-level expenditures and rolling up to condition based on each drug’s most likely indication. Some conditions were filtered out due to a lower fill volume.
The 2023 USDA Rural-Urban Continuum Codes were used to assign counties into either urban (RUCC code: 1-3) or rural counties (RUCC code: 4-10). The 2020 USDA rural-Urban Commuting Area was used to assign zip codes into either urban or rural using the same classification.
This story was produced by GoodRx and reviewed and distributed by Stacker.
![]()



